Dietitian Blog, MNT Guidelines | Jan 29 2020
Calciphylaxis: A lesser known complication of CKD
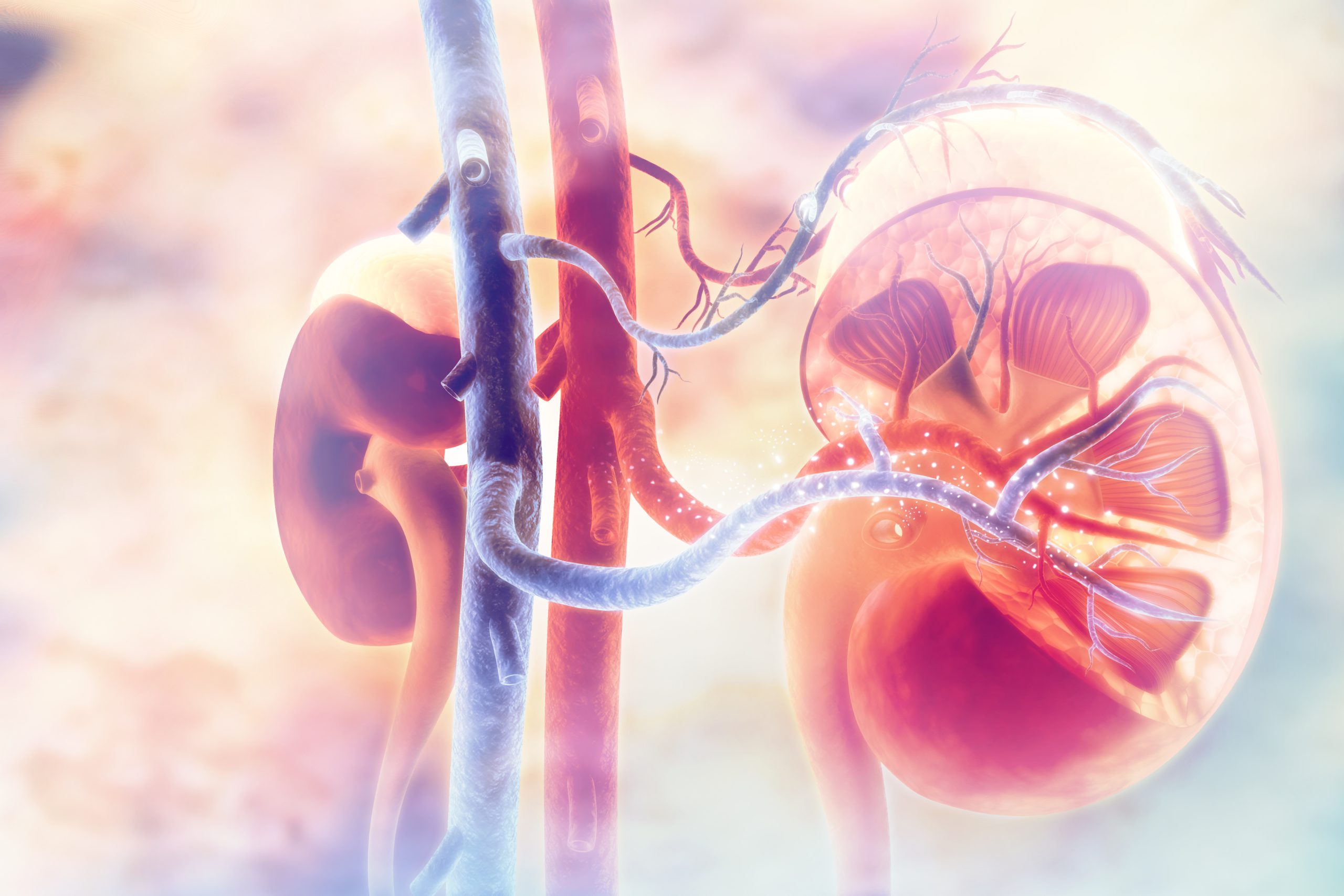
Normal kidney function supports strong bone health with the activation of vitamin D to help regulate balance of the body’s calcium, phosphorus, and parathyroid hormone (PTH). With chronic kidney disease, these levels can become imbalanced leading to bone and mineral disorders such as calciphylaxis.
What is calciphylaxis?
Calcific uremic arteriolopathy, more commonly known as calciphylaxis, is a rare vascular disease affecting less than 200,000 individuals in the United States per year. This disorder presents most commonly in individuals with kidney failure but can also be non-uremic in cause. Rather than being stored in the bones, calcium and phosphorus deposits collect in the small blood vessels of tissues in the fat and skin resulting in infection, blood clots and extremely painful skin ulcerations.
Symptoms of calciphylaxis can present differently in patients and include an abnormal purple skin pattern, painful skin lumps that open to ulcerations and poorly healing wounds. Diagnosis of calciphylaxis involves x-ray imaging, blood tests to assess kidney and liver function and a skin biopsy. Treatment is based on the individual and may require a combination of medication, hyperbaric oxygen therapy, dialysis, parathyroid gland surgery and intensive wound care depending on the patient. Despite intervention, the mortality rate for this disorder is as high as 50% after one year.
RD intervention: Role of MNT
With the complexity of calciphylaxis, management of diet with mineral and bone disease should be an early focus of medical nutrition therapy (MNT) intervention by the registered dietitian. According to the Kidney Disease Outcomes Quality Initiative (KDOQI) Guidelines, vitamin D, PTH, calcium and phosphorus levels should all be monitored. Based on laboratory values, medication, nutrient supplementation or diet modifications may be recommended. Understanding the basics of these values is essential in providing effective MNT.
Vitamin D: As kidney function declines, the kidneys are unable to convert vitamin D into an active form which triggers altered calcium, phosphorus and PTH. Vitamin D supplementation may be prescribed to reduce these alterations and monitored for appropriate dosing, lab values and side effects.
PTH: The parathyroid hormone regulates calcium in the body. If calcium levels drop, PTH production increases and pulls calcium from the bones into the blood. If calcium levels are too high, PTH may be overproduced and in severe cases may require parathyroid hormone surgery. Experts recommend regular monitoring of PTH, especially in more advanced kidney failure.
Calcium: Calcium is a primary component of the bones and regulated by PTH and availability of active vitamin D. Treatment for hypocalcemia involves vitamin D and calcium supplementation. In cases of hypercalcemia, the registered dietitian should ensure the patient isn’t consuming too many calcium-rich foods.
Phosphorus: This nutrient is also an important factor in bone health but as kidney function worsens, phosphorus is unable to effectively be filtered from the body. Depending on the stage of kidney disease, dialysis, diet and phosphorus binders can all help to maintain a normal phosphorus level. In regard to diet, the patient should be instructed to reduce phosphorus intake, especially sources of inorganic phosphorus (i.e., food preservatives) because of increased and harmful absorption.
Dietitians On Demand is a nationwide staffing and recruiting company for registered dietitians, specializing in short-term, temporary and permanent-hire positions in acute care, long term care and food service positions. We’re dedicated to dietitians and helping them enhance their practice and excel in the workplace. Check out our job openings, request your coverage, or visit our store today!
References
National Kidney Foundation: Mineral and Bone Disorder. https://www.kidney.org/atoz/content/MineralBoneDisorder. Updated June 2014. Accessed January 4, 2020.
Mayo Clinic: Calciphylaxis. https://www.mayoclinic.org/diseases-conditions/calciphylaxis/symptoms-causes/syc-20370559. Updated June 8, 2018. Accessed January 11, 2020.
Nigwekar SU. Calciphylaxis. Curr Opin Nephrol Hypertens. 2017;26(4):276–281. doi:10.1097/MNH.0000000000000328.
National Institute of Diabetes and Digestive and Kidney Diseases. Mineral and Bone Disorder in Chronic Kidney Disease. https://www.niddk.nih.gov/health-information/kidney-disease/mineral-bone-disorder. Updated November 2015. Accessed January 11, 2020.
Byham-Gray L, Stover J, Wiesen K. Clinical Guide to Nutrition Care in Chronic Kidney Disease. 2nd Chicago, IL: Academy of Nutrition and Dietetics;2013.
National Kidney Foundation: Bone, Calcium, Phosphate, and PTH in Kidney Failure. https://www.kidney.org.uk/bones-calcium-phosphate-and-pth-in-kidney-failure. Updated March 7, 2019. Accessed January 11, 2020.
Who we are
Dietitians On Demand is the nationwide leader in providing dietitians with jobs they love. If flexibility, competitive pay, a full benefits package, free CPEUs each month and a team dedicated to dietitians sound good to you, apply to our positions today.




