Dietitian Blog, MNT Guidelines, Nutrition Support | Oct 28 2020
Considerations for feeding acute care patients with spinal and head trauma
TBI vs SCI
A traumatic brain injury (TBI) can be defined as either a closed head injury or a penetrating injury, both resulting in disruption of the normal physiology of the brain.1 A closed head injury would involve a blow, bump, or jolt to the head, whereas a penetrating injury is caused when an object pierces the skull and enters brain tissue.1-2 Depending on the severity of damage, a patient’s symptoms can be classified as either mild, moderate, or severe.2 Critically ill patients with a TBI tend to have a multitude of other injuries, leading to a hypermetabolic, catabolic state that is present at the time of the injury.3-4
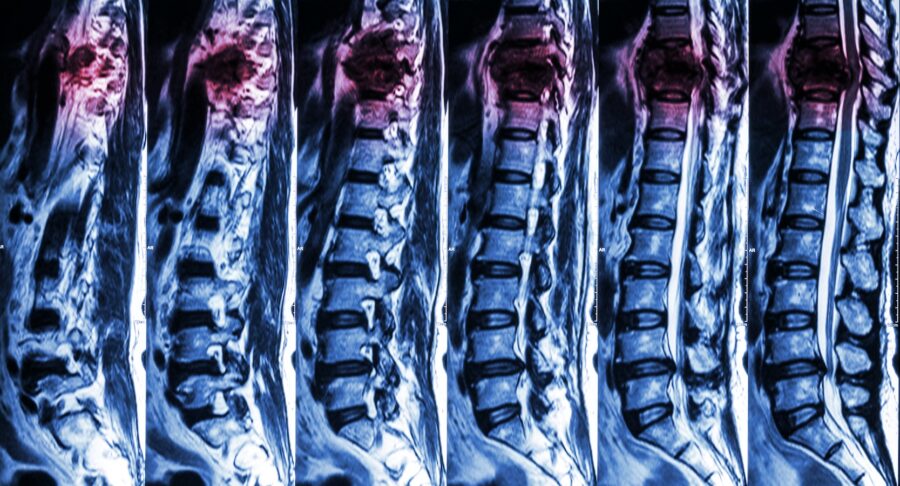
A spinal cord injury (SCI) is normally caused by a sudden, traumatic blow to the spinal cord resulting in a loss of function.5-6 After a SCI, mobility, sensations, and body organ functions can be affected below the level of the injury.6-5 The two main types of SCI are complete or incomplete injury.7 A complete injury can occur at any part of the spinal cord causing complete loss of function below the level of injury, equally affecting both sides of the body.7 An incomplete injury can also occur at any part of the spinal cord; however, some functions are still possible below the level of the injury, such as more movement in one limb compared to the other side, sensations in parts of the body, or more functionality on one side of the body.7
Timing and route of nutrition support
For a patient suffering from a TBI, initiation of nutrition support within the first 24 to 72 hours of the injury has shown to reduce mortality when compared to patients starting nutrition support on days three to five of hospitalization.3-4 Furthermore, research has shown that TBI patients had a two- and four-fold increased likelihood of death if nutrition was withheld the first five to seven days after the injury.3 No significant outcomes were noted when comparing TBI patients receiving parenteral nutrition (PN) over enteral nutrition (EN).3-4 However, EN should be the first line of action over PN due to its ability to maintain gut integrity, preserve gut-associated and mucosae-associated lymphoid tissues (GALT and MALT), and its cost-effectiveness.3-4 But as mentioned earlier, if the patient does not tolerate EN then it is in the best interest of the patient to start PN within a timely manner, due to the known benefits of early initiation of nutrition support for a TBI.3
At this time, no data is available to suggest that starting nutrition support within the first 72 hours after a SCI will improve neurologic status; however, there has been no proven negative effects to initiating early EN either.3 Patients with a SCI may have autonomic dysfunctions resulting in a paralytic ileus or neurogenic bowel.3 Both of these complications may hinder utilizing EN and will need to be evaluated on a case-by-case basis.
Energy needs
For patients with a TBI, energy requirements are impacted by other existing injuries (e.g., broken limbs, etc.), severity of the TBI, and medications.3 All of these factors can cause energy expenditure to vary between 87% and 200%.3 Indirect calorimetry (IC) is the gold standard; however, that is not always an available option for registered dietitians. The Brain Trauma Foundation, American Association of Neurological Surgeons, and Congress of Neurological Surgeons all recommend using 140% of what the Harris-Benedict equation predicts.3 A 2003 review done by the Academy of Nutrition and Dietetics found that the Harris-Benedict equation tends to overestimate resting metabolic rate and that other equations were more accurate. However, the Harris-Benedict equation has been the most studied predictive equation in TBI literature, so it continues to be utilized among this patient population.3 Protein requirements have a broad range at 1.5 to 2.5 g/kg/d.4
At this time, there is no predictive equation that has been validated for best use in patients with a SCI.3 Just as with a TBI, IC is the top choice when determining energy needs. One small study comparing seven SCI patients to seven severe TBI patients found that patients with a SCI had on average 48% lower energy needs when compared to the severe TBI patients.8 The higher the injury was in the spinal cord, the lower the measured resting energy expenditure (REE).3 Furthermore, REE was lower in patients with a complete SCI than those with an incomplete SCI.3 In the acute stages of a SCI, protein requirements have been estimated at 1.5 to 2 g/kg/d.3
When it comes to nutrition support both injuries are complex and have differing needs. Utilizing these guidelines can help RDs navigate their course of action when treating patients with TBI or SCI. As always, let clinical judgment help guide you through the process.
Dietitians On Demand is a nationwide staffing and recruiting company for registered dietitians, specializing in short-term, temporary and permanent-hire positions in acute care, long term care and food service positions. We’re dedicated to dietitians and helping them enhance their practice and excel in the workplace. Check out our job openings, request your coverage, or visit our store today!
References
Medline Plus: Traumatic Brain Injury. https://medlineplus.gov/traumaticbraininjury.html. Accessed August 13, 2020.
National Institute of Neurological Disorders and Stroke: Traumatic Brain Injury Information Page. https://www.ninds.nih.gov/Disorders/All-Disorders/Traumatic-Brain-Injury-Information-Page. Accessed August 13, 2020.
Mueller CM, Lord LM, Marian M, McClave SA, Miller SJ. The ASPEN Adult Nutrition Support Core Curriculum. 3rd Silver Spring, MD: American Society for Parenteral and Enteral Nutrition;2017.
McClave SA, Taylor BE, Martindale RG, et al. Guidelines for the provision and assessment of nutrition support therapy in the adult critically ill patient: Society of Critical Care Medicine (SCCM) and American Society for Parenteral and Enteral Nutrition (A.S.P.E.N.). JPEN J Parenter Enteral Nutr. 2016;40(2): 159-211.
National Institute of Neurological Disorders and Stroke: Spinal Cord Injury Information Page. https://www.ninds.nih.gov/Disorders/All-Disorders/Spinal-Cord-Injury-Information-Page. Accessed August 13, 2020.
Shepherd Center: Spinal Cord Injury Information. https://www.shepherd.org/patient-programs/spinal-cord-injury/about. Accessed August 13, 2020.
Columbia University Medical Center: Spinal Cord Injury. https://www.cumc.columbia.edu/rehab/staywell/document.php?id=34187. Accessed August 13, 2020.
Kolpek JH, Ott LG, Record KE, et al. Comparison of urinary urea nitrogen excretion and measured energy expenditure in spinal cord injury and nonsteroid-treated severe head trauma patients. JPEN J Parenter Enteral Med. 1989; 13(3):277-280.
Who we are
Dietitians On Demand is the nationwide leader in providing dietitians with jobs they love. If flexibility, competitive pay, a full benefits package, free CPEUs each month and a team dedicated to dietitians sound good to you, apply to our positions today.




