Dietitian Blog, Long-Term Care, MNT Guidelines | Apr 5 2021
How to complete section K of MDS 3.0 – A long-term care dietitian’s survival guide

If you have not worked with the MDS before, it can be very confusing to know how and what to document. We will review Section K of the MDS 3.0 and learn how to properly assess the resident and ensure the MDS is completed accurately.
As seen below, the items in this section are intended to assess the many conditions that could affect the resident’s ability to maintain adequate nutrition and hydration. This section covers swallowing disorders, height and weight, weight loss, and nutritional approaches. Dietitians should collaborate with the nursing and dietary staff to ensure that items in this section have been assessed and calculated accurately.
![]()
K0100: Swallowing Disorder
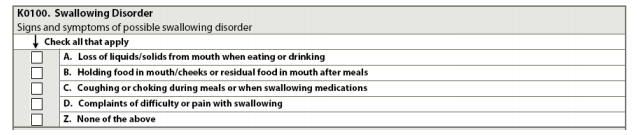
Steps for Assessment
1. Ask the resident if he or she has had any difficulty swallowing during the 7-day look-back period. Ask about each of the symptoms in A through D. Observe the resident during meals or at other times when he or she is eating, drinking, or swallowing to determine whether any of the listed symptoms of possible swallowing disorder are exhibited.
2. Interview staff members (any/all shifts) who work with the resident and ask if any of the four listed symptoms were evident during the 7-day look-back period.
3. Review the medical record, including nursing, physician, and speech language pathologist notes, to find any available information on dental history or problems. Dental problems may include poor fitting dentures, dental caries, edentulous, mouth sores, tumors and/or pain with food consumption
Coding Instructions (check all that apply)
- A, loss of liquids/solids from mouth when eating or drinking. When the resident has food or liquid in his or her mouth, the food or liquid dribbles down chin or falls out of the mouth.
- B, holding food in mouth/cheeks or residual food in mouth after meals. Holding food in mouth or cheeks for prolonged periods of time (sometimes labeled pocketing) or food left in mouth because resident failed to empty mouth completely.
- C, coughing or choking during meals or when swallowing medications. The resident may cough or gag, turn red, have more labored breathing, or have difficulty speaking when eating, drinking, or taking medications. The resident may frequently complain of food or medications “going down the wrong pipe.”
- D, complaints of difficulty or pain with swallowing. Resident may refuse food because it is painful or difficult to swallow.
- Z, none of the above: if none of the A through D signs or symptoms were present during the look-back.
*Note: In some facilities, another discipline (such as a SLP) may be responsible for coding the Swallowing Disorder section. Consult the MDS Coordinator to determine which discipline is responsible for MDS completion.
K0200: Height and Weight
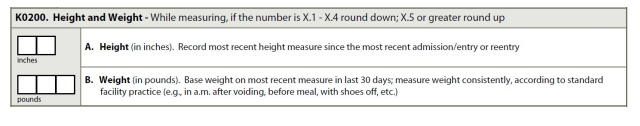
Steps for Assessment (Height)
- Base height on the most recent height since the most recent admission/entry or re-entry. Measure and record height in inches.
- Measure height consistently over time in accordance with the facility policy and procedure (shoes off, etc.).
- For subsequent assessments, check the medical record. If the last height recorded was more than one year ago, measure and record the resident’s height again.
Coding Instructions (Height)
- Record height to the nearest whole inch.
- Use mathematical rounding (i.e., if height measurement is X.5 inches or greater, round height upward to the nearest whole inch. If height measurement number is X.1 to X.4 inches, round down to the nearest whole inch).
Steps for Assessment (Weight)
- On admission, weigh the resident and record results.
- For subsequent assessments, check the medical record and enter the weight taken within 30 days of this assessment.
- If the last recorded weight was taken more than 30 days prior to the ARD of this assessment or previous weight is not available, weigh the resident again.
- If the resident’s weight was taken more than once during the preceding month, record the most recent weight.
Coding Instructions (Weight)
- Use mathematical rounding (i.e., If weight is X.5 pounds [lbs.] or more, round weight upward to the nearest whole pound. If weight is X.1 to X.4 lbs., round down to the nearest whole pound).
- If a resident cannot be weighed, for example because of extreme pain, immobility, or risk of pathological fractures, use the standard no-information code (-) and document rationale on the resident’s medical record.
K0300: Weight Loss
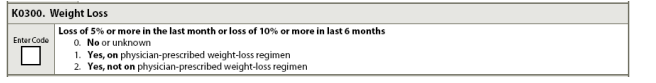
Steps for Assessment
This item compares the resident’s weight in the current observation period with his or her weight at two snapshots in time:
1. At a point closest to 30-days preceding the current weight.
2. At a point closest to 180-days preceding the current weight.
Coding Instructions
- Code 0, no or unknown: if the resident has not experienced weight loss of 5 percent or more in the past 30 days or 10 percent or more in the last 180 days or if no prior weight is available.
- Code 1, yes on physician-prescribed weight loss regimen: if the resident has experienced a weight loss of 5 percent or more in the past 30 days or 10 percent or more in the last 180 days, and the weight loss was planned and pursuant to a physician’s order.
- Code 2, yes, not on physician-prescribed weight-loss regimen: if the resident has experienced a weight loss of 5 percent or more in the past 30 days or 10 percent or more in the last 180 days, and the weight loss was not planned and prescribed by a physician.
K0310: Weight Gain
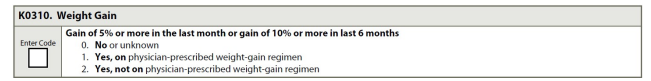
Steps for Assessment
This item compares the resident’s weight in the current observation period with his or her weight at two snapshots in time:
1. At a point closest to 30-days preceding the current weight.
2. At a point closest to 180-days preceding the current weight.
Coding Instructions
- Code 0, no or unknown: if the resident has not experienced weight gain of 5 percent or more in the past 30 days or 10 percent or more in the last 180 days or if no prior weight is available.
- Code 1, yes on physician-prescribed weight-gain regimen: if the resident has experienced a weight gain of 5 percent or more in the past 30 days or 10 percent or more in the last 180 days, and the weight gain was planned and pursuant to a physician’s order. In cases where a resident has a weight gain of 5 percent or more in 30 days or 10% or more in 180 days as a result of any physician ordered diet plan, K0310 can be coded as 1.
- Code 2, yes, not on physician-prescribed weight-gain regimen: if the resident has experienced a weight gain of 5 percent or more in the past 30 days or 10 percent or more in the last 180 days, and the weight gain was not planned and prescribed by a physician.
K0510: Nutritional Approaches
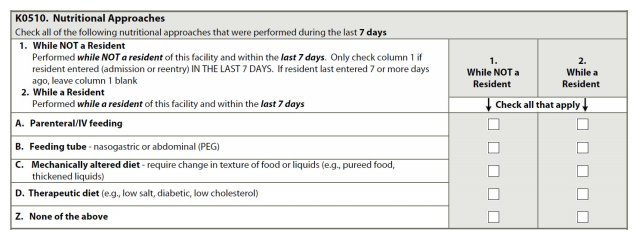
Steps for Assessment
- Review the medical record to determine if any of the listed nutritional approaches were received by the resident during the 7-day look-back period. This includes any and all nutrition and hydration received by the resident in the last 7 days either at the nursing home, at the hospital as an outpatient or an inpatient, provided they were administered for nutrition or hydration.
Coding Instructions (check all that apply)
- A, parenteral/IV feeding
- B, feeding tube – nasogastric or abdominal (PEG)
- C, mechanically altered diet – require change in texture of food or liquids (e.g., pureed food, thickened liquids)
- D, therapeutic diet (e.g., low salt, diabetic, low cholesterol)
- Z, none of the above
K0710: Percent Intake by Artificial Route
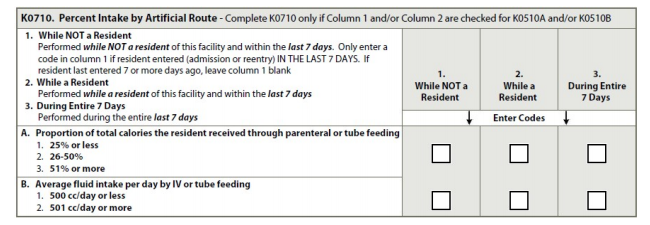
* Complete K0710 only if Column 1 and/or Column 2 are checked for K0510A and/or K0510B
K0710A, Proportion of Total Calories the Resident Received through Parental or Tube Feeding
Steps for Assessment
- Review intake records to determine actual intake through parenteral or tube feeding.
- Calculate proportion of total calories received through these routes.
- If the resident took no food or fluids by mouth or took just sips of fluid, stop here and code 3, 51% or more.
- If the resident had more substantial oral intake than this, consult with staff.
Coding Instructions
- Select the best response:
- 25% or less
- 26% to 50%
- 51% or more
K0710B, Average Fluid Intake per Day by IV or Tube Feeding
Steps for Assessment
1. Review intake records from the last 7 days.
2. Add up the total amount of fluid received each day by IV and/or tube feedings only.
3. Divide the week’s total fluid intake by 7 to calculate the average of fluid intake per day.
4. Divide by 7 even if the resident did not receive IV fluids and/or tube feeding on each of the 7 days.
Coding Instructions
Code for the average number of cc’s of fluid the resident received per day by IV or tube feeding. Record what was actually received by the resident, not what was ordered.
- Code 1: 500 cc/day or less
- Code 2: 501 cc/day or more
This is the second part in a MDS 3.0 series.
Read part 1 here!
Dietitians On Demand is the nationwide leader in staffing registered dietitians, specializing in short-term, temporary and permanent-hire positions in acute care, long term care and food service positions. Our dietitians cover a vacancy, maternity leave, vacations, FMLA or increases in census. Check out our job openings, or request your coverage today!
Who we are
Dietitians On Demand is the nationwide leader in providing dietitians with jobs they love. If flexibility, competitive pay, a full benefits package, free CPEUs each month and a team dedicated to dietitians sound good to you, apply to our positions today.