Dietitian Blog, Nutrition Support | Jul 19 2022
Managing refeeding syndrome in parenteral nutrition

Parenteral nutrition (PN) allows clinicians to patients’ nutritional needs when oral or enteral routes are not feasible. However, this nutrition therapy is typically reserved as a “last resort” and is not without risks. Many patients receiving PN are at risk for developing refeeding syndrome when nutrition support is restarted after a period of inadequate nutrition. Fortunately, this condition is preventable and treatable.
Refeeding syndrome occurs as the body adjusts from starvation and energy conservation to a state of anabolism. As exogenous fuel is reintroduced into the body, insulin production increases with the influx of carbohydrates. This in turn promotes increased intracellular and metabolic demands for nutrients – specifically potassium, magnesium, phosphorus, and thiamine. The resulting electrolyte and vitamin deficits can cause symptoms of cardiovascular, neuromuscular, and respiratory dysfunction.
Dietitians should be on alert for refeeding syndrome for all hospitalized patients. PN in particular poses inherent risks given the direct infusion of dextrose into the bloodstream. Furthermore, patients receiving PN may already be in a nutrition deficit from an overall delay in nutrition provision or failure of oral and enteral feeding regimens. Additionally, increased metabolic demands may mean increased carbohydrate goals to meet acute needs. The risk of refeeding syndrome in these patients should be evaluated prior to PN initiation, and close follow-up should be provided to ensure safe nutrition delivery.
Identifying patients at risk for refeeding syndrome
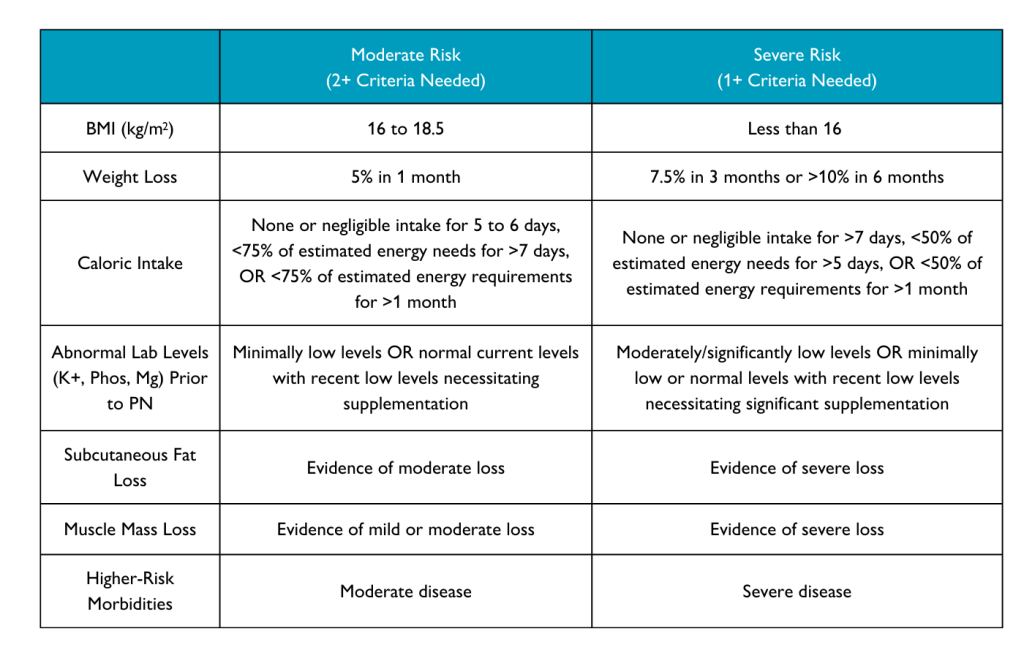
The American Society of Parenteral and Enteral Nutrition (ASPEN) describes the following criteria used to estimate an adult patient’s risk for developing refeeding syndrome:
Initiating and advancing parenteral nutrition
Calories, in particular carbohydrates, should be slowly introduced. An initial dose of 100 to 150 grams of dextrose per day or 10 to 20 calories/kilogram/day is generally considered safe for the first 24 hours. If phosphorus, potassium, and magnesium levels are stable, slow advancement to goal dextrose is advised. ASPEN recommendations specify advancement of 33% of goal every one to two days, which generally equates to 50 to 100 grams of dextrose per day but may vary based on the patient’s nutritional needs and clinical acuity.
If phosphorus, potassium, and magnesium levels are unstable, dextrose advancement should be delayed. Since carbohydrates are the main macronutrient of concern with refeeding syndrome, slowly advancing other macronutrients to the goal amount can be considered if dextrose progress is stalled. Dextrose advancement can resume once electrolytes are adequately repleted and repeat levels are acceptable.
Electrolyte management
Since electrolyte shifts are a hallmark component of refeeding syndrome, it is pertinent to closely follow serum levels from the time of PN initiation until goal infusion is obtained. Potassium, magnesium, and phosphorus levels should be checked prior to proceeding with PN delivery. Monitor levels at least every 12 hours for the first three days in high-risk patients. Replete low electrolytes per established standards of care at your facility. If electrolytes become too difficult to correct or drop to unsafe levels, decrease to 50% of calories/grams of dextrose until the electrolytes of concern are within normal limits, then proceed with further advancement.
Thiamine and multivitamins
Thiamine is a cornerstone of glucose metabolism. Patients may be predisposed to a thiamine deficiency from poor nutrition status, or a thiamine deficiency may result from increased utilization during refeeding. Addition of thiamine to the nutrition regimen should be considered for both populations—individuals deemed at risk for refeeding syndrome and patients with a confirmed or suspected deficiency.
Supplementation with 100 mg of thiamine before infusing PN or any dextrose-containing intravenous fluids is advised. Once added, supplementation should then continue as part of the PN prescription for at least five to seven days until refeeding syndrome has subsided but can be continued for those who still exhibit signs of refeeding syndrome or other thiamine-depleted states. Unless contraindicated, ensure a daily multivitamin is included in the nutrition interventions to address other vitamin and mineral needs.
Monitoring and long-term care
A multidisciplinary approach is needed to comprehensively monitor refeeding patients. Discuss concerns regarding refeeding risk with your medical team. This will help ensure that vitals, labs, and patient monitoring are sufficient. With ample risk identification and smart nutrition interventions, avoidance and treatment of refeeding syndrome are attainable.
Dietitians On Demand is a nationwide staffing and recruiting company for registered dietitians, specializing in short-term, temporary and permanent-hire positions in acute care, long term care and food service positions. We’re dedicated to dietitians and helping them enhance their practice and excel in the workplace. Check out our job openings, request your coverage, or visit our store today!
References:
Da Silva JS, Seres DS, Sabino K, et al. Aspen Consensus Recommendations for Refeeding Syndrome. Nutrition in Clinical Practice. 2020;35(2):178-195. doi:10.1002/ncp.10474
Kumpf VJ, Gervasio J. Complications of Parenteral Nutrition. In: The ASPEN Adult Nutrition Support Core Curriculum. 3rd ed.; 2017:345-360.
Who we are
Dietitians On Demand is the nationwide leader in providing dietitians with jobs they love. If flexibility, competitive pay, a full benefits package, free CPEUs each month and a team dedicated to dietitians sound good to you, apply to our positions today.




