Dietitian Blog, Long-Term Care, MNT Guidelines, Nutrition Support | Apr 25 2022
The ultimate nutrition support guide for dietitians
What is nutrition support?
Nutrition support includes enteral and parenteral nutrition, known by many clinicians as tube feeding and TPN. Tube feeding is utilized any time the GI tract is functional, but an individual cannot safely eat, drink, or meet their nutritional needs by mouth. Dietitians often use enteral nutrition for patients with dysphagia, those on a mechanical ventilator, and even for pediatric patients who may have feeding difficulties.
On the other hand, parenteral nutrition is used when the GI tract is not functional. Parenteral nutrition is also called TPN, and it delivers nutrients and fluid directly to the bloodstream, bypassing the GI tract altogether. TPN is often used in the treatment of bowel obstructions, a paralytic ileus, intestinal failure (previously known as short bowel syndrome), and in the cases of severe malabsorption.
Although nutrition support allows for the most customizable nutrition regimens, some dietitians feel less-than-confident when it comes to crafting successful enteral and parenteral nutrition orders. But that doesn’t have to be the case. We’ve gathered all our best nutrition support resources right here in one place. Get your questions answered and raise your confidence level starting right now.
In this article:
- How to calculate a patient’s nutritional needs
- Getting to know the basics about tube types and formulas
- Selecting an enteral formula
- What are blenderized tube feeding formulas?
- What is the ENFit® connector?
- How volume-based feeding can benefit your patients
- Getting started with TPN
- Writing custom TPN orders
- Troubleshooting common nutrition support problems
How to calculate a patient’s nutritional needs
The first step to any successful tube feeding or TPN regimen is to estimate the patient’s calorie, protein, and fluid needs. As any dietitian knows, different medical conditions or life stages yield different nutritional needs.
Because calculations are different based on medical condition and life stage, it’s impossible for a dietitian to try and memorize them all. From pregnancy and breastfeeding to pressure injuries, burns, trauma, and kidney disease, it’s important to use the correct calculation.
We’ll include a few of the most common calculations here, but never fear, there’s a cheat sheet with calculations for over a dozen conditions.
CHRONIC KIDNEY DISEASE
Calories:
- Stage 3 to 5D, hemodialysis, peritoneal dialysis: 25 to 35 kcal/kg
Protein:
Stage 3 to 5:
- Very low protein diet + keto acid analogs: 0.28 to 0.43 g/kg
- Low protein diet non-DM: 0.55 to 0.6 g/kg
- Low protein diet with DM: 0.6 to 0.8 g/kg
- Stage 5D, hemodialysis and peritoneal dialysis (with/without diabetes): 1.0 to 1.2 g/kg
- *Adjust protein provision based on metabolic stability
Fluid:
Stage 1 to 4: individualized based on comorbidities, physical findings, and alterations in urine output
Stage 5D, hemodialysis: urine output + 1,000 to 1,200 ml
Stage 5D, peritoneal dialysis: maintain fluid balance
CRITICALLY ILL
Calories:
BMI <30 kg/m2: 25 to 30 kcal/kg
BMI 30 to 50 kg/m2: 11 to 14 kcal/kg of actual weight
BMI >50 kg/m2: 22 to 25 kcal/kg of ideal weight
Protein:
BMI <30 kg/m2: 1.2 to 2 g/kg
BMI 30 to 40 kg/m2: 2 g/kg of ideal weight
BMI >40 kg/m2: 2.5 g/kg of ideal weight
PRESSURE INJURIES
Calories: 30 to 35 kcal/kg or 35 to 40 kcal/kg for patients losing weight
*Adjust energy based on weight change or level of obesity
Protein: 1.25 to 1.5 g/kg
Fluid: 30 ml/kg or 1 to 1.5 ml/kcal
SURGERY (MAJOR)
Calories: 30 to 35 kcal/kg
Protein: 1.5 to 2 g/kg
Read more: A complete cheat sheet on calculating energy needs
Getting to know the basics about tube types and formulas
There are several different kinds of feeding tubes. Some are meant for short-term use, while others can be used for several months or even years. Likewise, feeding tubes can deliver nutrition either to the stomach or small intestine.
Feeding tubes are named by how they are placed in the body and where the end of the tube is located in the body. For example, if someone has a tube placed through his/her nose and the end of the tube is located in their stomach, it is called a nasogastric tube (“naso” for nose and “gastro” for stomach).
Many patients receive tube feeding while receiving medical care in a hospital or long-term care facility. Individuals may safely utilize enteral nutrition as either sole source or supplemental nutrition at home, too. While commercially prepared formulas are available, blenderized or food-based formulas are becoming more popular and readily available as well. When it comes to choosing a formula, there are several considerations, which we’ll cover next.
Read more: Answers to the top 5 questions and misconceptions about feeding tubes
Selecting an enteral formula
After you have calculated your patient’s estimated energy needs, the next step is to choose an enteral formula. Most enteral formulas provide complete nutrition, including macro- and micronutrients.
There are a few different categories of enteral formulas. Standard polymeric formulas are used in most patients and provide a nutrient profile most similar to a typical oral diet. They may or may not contain fiber.
Semi-elemental or elemental formulas contain partially or fully hydrolyzed proteins and can be directly absorbed in the presence of GI dysfunction, such as malabsorption. Specialty formulas are designed to provide tailored medical nutrition therapy for specific disease states.
When choosing the best formula, consider a patient’s nutritional needs — do they need a higher protein formula, one that is fluid restricted, or one with specific nutrients restricted? Next, think about GI function — is there a need for a partially hydrolyzed formula or unique fiber needs? And finally, are there insurance or payment concerns that may factor into your decision?
Read more: A full enteral nutrition overview
What are blenderized tube feeding formulas?
Blenderized, food-based tube feeding formulas may be foreign to many dietitians. However, they have been increasing in popularity in the last few years. There are several commercially produced blenderized formulas on the market, most made with whole food ingredients. Alternatively, patients or caregivers may wish to pursue a homemade blenderized formula.
Nearly any patient can be a good candidate for a blenderized formula. When deciding to go this route, there are some additional details to consider. First, consider whether a patient will be using an enteral feeding pump. Blenderized formulas often need to be diluted or thinned to be compatible with feeding pumps. Also, make sure the patient’s micronutrient needs are met.
Commercially prepared blenderized formulas may not provide 100% of a patient’s vitamin and mineral needs; the same is true for homemade recipes. And finally, educate your patient or client on food safety practices, particularly when using a homemade blenderized formula.
Read more: Exploring food-based formulas
What is the ENFit® connector?
The hardware on feeding tubes and supplies has recently changed to a new connector called called ENFit®. This change is part of an international patient safety effort. Previously, the same Luer-type (also known as Legacy or “Christmas tree”) syringes and connectors could be used with both IV tubing and feeding tubes, creating the potential for serious medical errors. ENFit® utilizes a notched design and twisting mechanism to ensure that enteral formula can only be infused into an enteral feeding tube.
Most enteral nutrition equipment and suppliers have fully transitioned to the new ENFit® tubing. However, dietitians should be aware that they may still encounter the old Luer-type tubes with patients who have had a feeding tube in place for many years. In this case, ensure the patient has compatible enteral supplies and use an adapter, if needed.
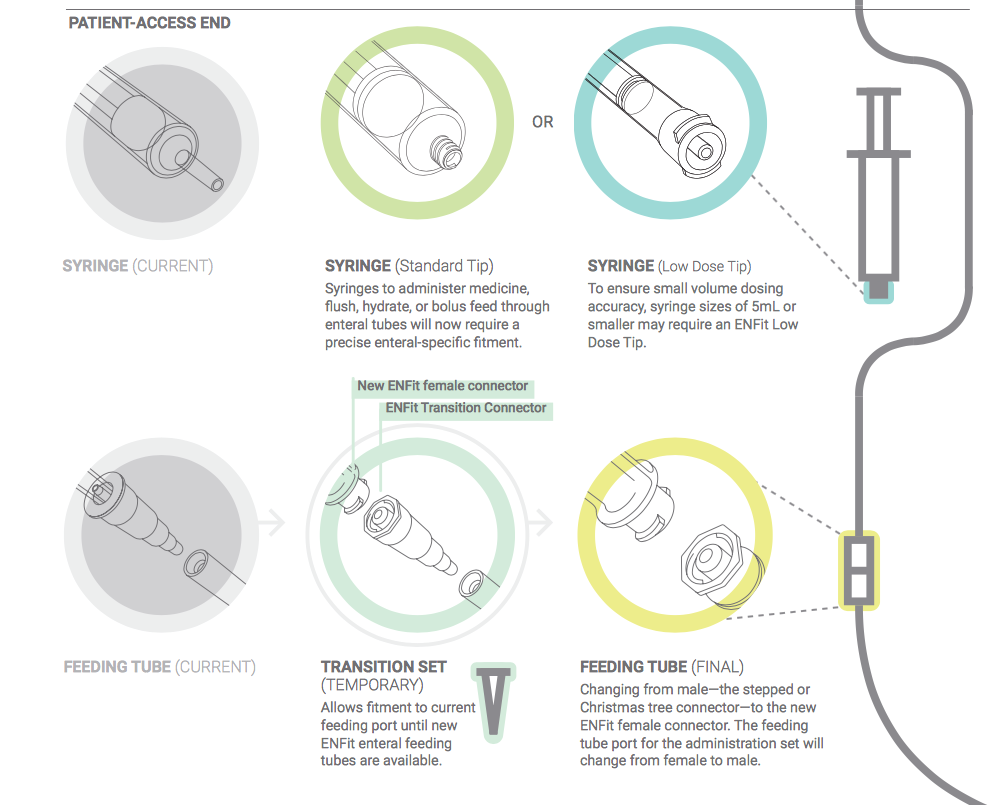
The image above demonstrates how ENFit® is different. Previously, the same Luer-type syringes and connectors could be used with both IV tubing and feeding tubes, creating the potential for serious errors. ENFit® utilizes a notched design and twisting mechanism to ensure that enteral formula can only be infused into an enteral feeding tube.
Read more: Learn more about ENFit®
How volume-based feeding can benefit your patients
Malnutrition and inadequate feedings are common challenges for dietitians in the critical care setting. Early initiation and adequacy of enteral feedings have been shown to provide numerous clinical benefits. This is especially true when it comes to patients in the ICU.
Volume-based tube feeding involves adjusting the infusion rate throughout the day so that a daily volume goal is achieved, rather than a goal infusion rate. Nurses are empowered to increase the enteral infusion rate to “catch up” if the tube feeding infusion is interrupted during the day. This approach helps to ensure the patient receives all the nutrients they need. The success of a volume-based feeding protocol depends heavily on interdisciplinary communication and cooperation.
Read more: What is volume-based feeding?
Getting started with TPN
Total parenteral nutrition is one of the most customizable and specialized, yet high-risk and intimidating nutrition therapies of them all. It’s a great option when patients really need it, but many dietitians don’t feel comfortable managing TPN.
The first step to using TPN is deciding whether it’s the best option for your patient. Because of the risks and cost associated with parenteral nutrition, it should be reserved for patients who have a non-functioning GI tract or cannot meet their nutritional needs with enteral nutrition alone.
It is reasonable to withhold TPN for up to seven days for well-nourished patients. However, patients who are malnourished or at high nutrition risk should begin TPN right away when other feeding plans fail.
When you have decided parenteral nutrition is the best option, estimate how long the patient is likely to need parenteral nutrition. This will help you decide whether peripheral or central IV access is needed. Peripheral parenteral nutrition (PPN) can be used as a short-term solution or bridge to supplement a patient’s nutritional needs. If the patient is likely to need parenteral nutrition for more than five days, they will likely need a central line to receive TPN and more fully meet their nutritional needs.
Writing custom TPN orders
In many healthcare facilities, dietitians have earned order-writing privileges, and this includes nutrition support. If your facility relies on dietitians to calculate and write custom TPN orders, there is a stepwise process to do so.
First, calculate the patient’s calorie, protein, and fluid needs. This will help guide you as you determine the macronutrient breakdown of the parenteral nutrition order.
Second, consider how much fluid the patient will need. Many times, all other sources of IV fluids are discontinued once a TPN infusion begins. You may wish to clarify this with the attending physician.
Typically, parenteral nutrition is infused over 24 hours, especially when a new order is beginning. Take your patient’s estimated fluid needs and divide it by 24 to determine the infusion rate of your TPN. It’s okay to round to the nearest whole number or even to the nearest five (e.g., 60, 65, 70, etc.).
Third, begin your macronutrient calculations. Start with amino acids, as protein is always a priority. This is also a simple calculation—add enough amino acids to match the patient’s protein needs. For example, if your patient needs 80 grams of protein per day, add 80 grams of amino acids to the TPN.
If you plan to add lipids to your parenteral nutrition order, calculate those next. Dose lipids similar to the acceptable macronutrient distribution range (AMDR) for fat—20% to 35% of total calorie needs from fat. It is generally reasonable to provide approximately 25% of total calories from lipids. To calculate this, you will multiply your patient’s estimated calorie needs by 25%, then divide by 10 to determine the number of grams needed. (Intravenous lipids provide 10 calories per gram, not nine.)
All remaining calories in the TPN will be provided by dextrose. Simply subtract the calories provided by amino acids and lipids from the patient’s estimated calorie needs. Your result is the number of calories that should be provided by dextrose. Dextrose provides 3.4 calories per gram, so divide your remaining calories by 3.4 to calculate how many grams of dextrose should be added to the TPN.
Most often, dietitians or pharmacists manage the electrolytes in a TPN. This is often a complex process and highly customized to each individual patient.
Troubleshooting common nutrition support problems
Even the most well-crafted nutrition support regimens can be plagued with complications or intolerance. However, many of these complications can be prevented or managed.
With enteral nutrition, the most common complications are often a clogged feeding tube or GI intolerance. If you are coping with a clogged tube, start by instilling warm water into the tube and manually squeezing or pinching the outside of the tube to break up any clogs. There are also several commercial declogging agents or devices that work well. If GI intolerance is an issue, try to rule out other causes of nausea, high gastric residual volumes, or diarrhea. Oftentimes, the tube feeding regimen is unnecessarily blamed when there may be another culprit.
With parenteral nutrition, complications are often more serious or can escalate quickly. Lab abnormalities, especially hyperglycemia, are common. If your patient is hyperglycemic with blood glucose readings consistently above 180 mg/dl, speak with the attending physician and pharmacist about adding or adjusting the patient’s insulin regimen. If lab abnormalities are due to refeeding syndrome, it’s important to replete low electrolytes as soon as possible outside the TPN bag. Avoid increasing levels of dextrose in the TPN until potassium, phosphorus, and magnesium labs are stable.
Read more: Troubleshooting common nutrition support problems
Dietitians On Demand is a nationwide staffing and recruiting company for registered dietitians, specializing in short-term, temporary and permanent-hire positions in acute care, long term care and food service positions. We’re dedicated to dietitians and helping them enhance their practice and excel in the workplace. Check out our job openings, request your coverage, or visit our store today!
Who we are
Dietitians On Demand is the nationwide leader in providing dietitians with jobs they love. If flexibility, competitive pay, a full benefits package, free CPEUs each month and a team dedicated to dietitians sound good to you, apply to our positions today.