Dietitian Blog, Long-Term Care, MNT Guidelines | May 17 2021
The importance of an individualized care plan in long-term care settings

Medical record documentation has always been a critical component in the healthcare/medical field, and this is especially true in long-term care settings. Proper documentation is required to support MDS coding, reimbursement, and the need for skilled services on an inpatient basis.
Documentation has become increasingly difficult as the resident’s clinical needs are more complex, regulations and surveys are more stringent, litigations/legal challenges have increased, and documentation-based payment systems have been implemented.
Federal regulation requires that a facility, “must maintain clinical records on each resident in accordance with accepted professional standards and practices that are complete, accurately documented, readily accessible and systematically organized.”
Medicare charting in long-term care
Medicare charting is necessary for the confirmation of services needed for continuation of skilled care. Most facilities divide the charting between day and evening shift in a 24-hour period. The charting should include vital signs, why the resident is receiving skilled services, and a detailed description of the resident’s condition at that time.
The four pillars of medicare charting include:
- Inherent Complexity
- Observation and Assessment
- Management and Evaluation of a Care Plan
- Teaching and Training
Why is the Resident Care Plan important?
Of the four pillars of Medicare charting, the care plan is unique in that it often involves multiple disciplines and in its ideal state should become each resident’s unique path toward achieving or maintaining his/her highest practicable level of well-being.
Currently, most facilities involve multi-disciplines in the management and evaluation of the care plan, such as social work, physical therapy, occupational therapy, speech language pathology, pharmacy, and nutrition/dietary. The care plan allows the team to be on the same page and work towards a collaborative goal.
For example, if the goal is: “prevention of pressure ulcers,” it can be identified under the nursing care plan as well as under other members of the health care team. Overall, this interdisciplinary focus tends to foster a more holistic approach to resident care and strengthens team communication.
The care plan also serves as a guide for reimbursement and at times will be used by the insurance companies to determine what they will pay in relation to the care received by the resident. State and federal surveyors often look at the care plan during their visits to make sure that they are being done on and individualized basis and being updated consistently.
What should the care plan include?
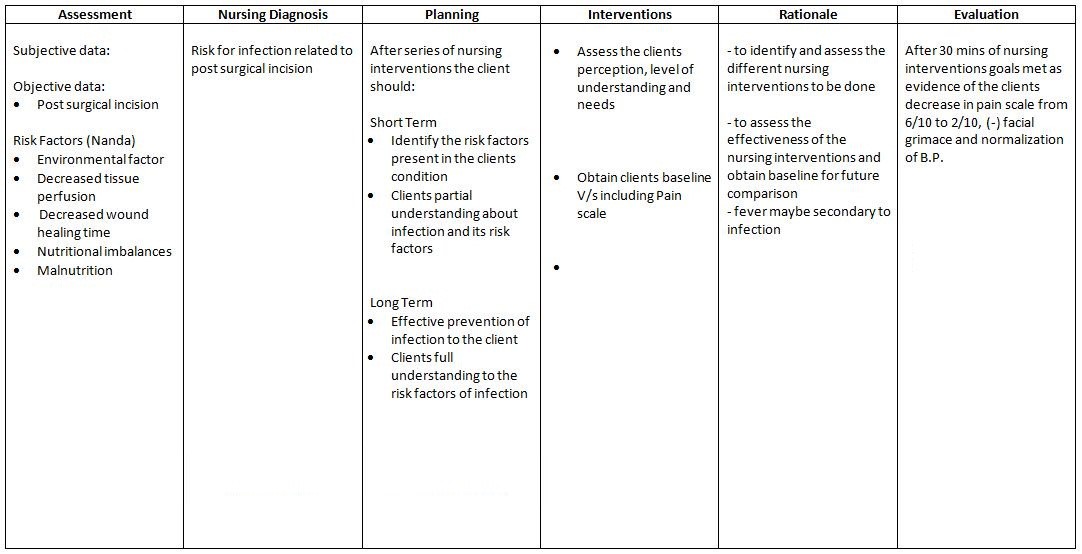
An example of a standard care plan for the long-term care setting.
- Each member of the interdisciplinary team should have an individual category, or an area within the resident’s care plan to document independently
- List the resident’s unique diagnoses and organize them by the individual’s specific needs
- The information should give a clear picture of the plan to improve a resident’s health needs — and your interventions (nutritional supplements, wound healing vitamin regimen, etc.)
- The reason or rationale behind your specified interventions
- How you plan to monitor/evaluation this — specified time frames are best (i.e. within this quarter, within the next 30 days, etc.)
- It should be updated every time you complete an assessment or document on the resident — this also helps the facility track changes in the resident’s status throughout their stay
The individualized care plan can provide powerful and persuasive resident outcomes in terms of their quality of care and quality of life. When a facility has a care plan that reflects their individual problems and causes, linked with the appropriate resident-specific approaches to care, it has been shown that the resident’s level of functioning has improved or declined at a slower rate.
References:
Documentation in the Long-Term Care Record. 2014. American Health Information Management Association. http://ahimaltcguidelines.pbworks.com/w/page/46508844/Documentation%20in%20the%20Long%20Term%20Care%20Record. Accessed November 10, 2018.
Lewis, L. Documentation Guidelines for Skilled Care. 2017. PHCA. http://www.pacahpa.org/Education/DocumentationGuidelinesforSkilledCarePACAH.pdf. Accessed November 10, 2018.
Mastrangelo, K. 2016. Skilled Nursing Documentation (Part One): The Four Pillards. Harmony Healthcare. http://htpp//www.harmony-healthcare.com/blog/how-to-document-daily-skilled-nursing-services-in-the-medicare-post-acute-setting. Accessed November 12, 2018.
Who we are
Dietitians On Demand is the nationwide leader in providing dietitians with jobs they love. If flexibility, competitive pay, a full benefits package, free CPEUs each month and a team dedicated to dietitians sound good to you, apply to our positions today.




