Dietitian Blog, MNT Guidelines | Sep 3 2019
Diagnosing food allergies: What every dietitian needs to know
Food allergies are on the rise. According to the Food Allergy Research and Education (FARE) organization, the prevalence of food allergies has increased by 50 percent between 1997 and 2011, while the prevalence of peanut and tree nut allergies has tripled between 1997 and 2008.1
Having a food allergy limits food choices and may even impact nutritional health and quality of life. As such, it’s important that reported food allergy symptoms are confirmed with diagnostic tests, so that foods are not restricted unless absolutely necessary.
What qualifies as a true food allergy?
Sometimes, food intolerances or any type of reaction associated with food is mislabeled an “allergy” without any formal diagnosis. In the vernacular, the term “allergy” can refer to any food that causes a reaction. However, food allergies trigger true immune system responses when they are consumed.
This immune response is specific to each individual and results in the same symptoms after each exposure to the allergen. Food intolerances can also cause the same reaction when eaten, but the body’s response is not from the immune system.
Food allergy diagnostic tests
Currently, physicians use skin tests, prick-to-prick tests, patch tests, and blood tests to begin diagnosing a food allergy. However, none of these methods stand alone for a diagnosis. These test results must be considered with the patient’s medical history and must be confirmed by an oral challenge — the gold standard in diagnosing a food allergy. Let’s review the diagnostic tests that are most often used.
Skin tests
Skin tests are often the first test utilized when starting the process to diagnose a food allergy. Skin tests are designed to look for the immunoglobulin E (IgE) response on the skin’s mast cell. Under the umbrella of skin tests, there are three different techniques: prick tests, scratch tests, and intradermal tests.
In a prick test, a drop of the allergen extract is placed onto the skin, and the skin underneath is pricked. In a scratch test, the skin is scratched and a drop of the allergen is placed on the scratch. In an intradermal test, the allergen is injected into the skin from a syringe. After a short waiting period, the skin’s reaction is interpreted to determine if an immune response is suspected.
Prick-to-prick tests
Prick-to-prick tests are similar to skin prick tests; however, they use raw foods instead of commercial allergen solutions. In this test, a needle is inserted into the raw food and the skin is pricked with that same needle. The skin’s reaction determines if an allergy is suspected.
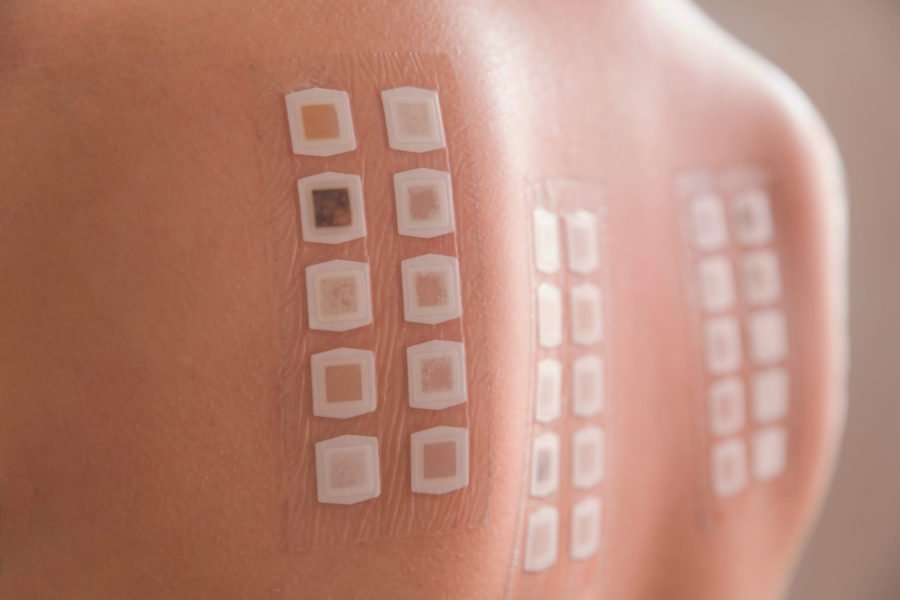
Patch tests
These tests do not involve a scratch or needle prick. Instead, clinicians place a patch with the allergen on the surface of the skin and monitor for a reaction.
Blood tests
No single lab test is available to assess specific food reactions for all types of immune responses. Blood tests commonly used are looking for immunoglobulin G (IgG) or IgE response, both specific immune responses. IgE tests include the radioallergosorbent test (RAST) and fluorescent allergosorbent test (FAST). IgG testing includes enzyme-linked immunosorbent assay (ELISA).
Gold standard: The oral challenge
The oral challenge is currently the gold standard for diagnosing a food allergy and is required to confirm the suspected diagnosis from any other allergy test.
In the oral challenge, the suspected food is removed for a period of time during an elimination diet, then reintroduced back into the diet. If symptoms are present after the food is reintroduced, then an allergy diagnosis is confirmed.
This process varies based on the severity of the suspected allergic reaction, how many foods are suspected to cause an allergic response, and previous allergy testing results. An oral food challenge should not be attempted independently, but either under physician supervision or with physician approval.
The process for diagnosing a food allergy is long and multi-faceted. Those who have undergone this process know with confidence what their food allergies are and how their body responds.
Although a person can have reactions to foods that seem similar to allergic reactions, these reactions are not considered true food allergies unless they are diagnosed as an immune response. Dietitians can play important roles in both the diagnostic process and education phase once allergies are confirmed.
Dietitians On Demand is a nationwide staffing and recruiting company for registered dietitians, specializing in short-term, temporary and permanent-hire positions in acute care, long term care and food service positions. We’re dedicated to dietitians and helping them enhance their practice and excel in the workplace. Check out our job openings, request your coverage, or visit our store today!
References
Food Allergy Research & Education. (2019, February). Facts and Statistics. Retrieved from https://www.foodallergy.org/life-with-food-allergies/food-allergy-101/facts-and-statistics.
Joneja, J.V. (2013). The Health Professional’s Guide to Food Allergies and Intolerances. Chicago, Illinois; Academy of Nutrition and Dietetics.
Who we are
Dietitians On Demand is the nationwide leader in providing dietitians with jobs they love. If flexibility, competitive pay, a full benefits package, free CPEUs each month and a team dedicated to dietitians sound good to you, apply to our positions today.




